Am Heart J, 102 Aug;124(2):544-9
Magnesium deficiency and sudden death
Mark J. Eisenberg, MD, MPH San Francisco,
Calif.
Over the past three decades, a variety of epidemiologic,
autopsy, clinical, and animal studies have suggested an
association between magnesium (Mg) deficiency and sudden death.
This association may have far-reaching implications, because
sudden death continues to be a major cause of cardiovascular
mortality in the United States and accounts for over 300,000
deaths per year.1, 2 Early studies showed an inverse
relationship between drinking water content and cardiovascular
disease incidence,3, 4 but much of this relationship
was subsequently shown to be the result of an association between
water hardness and sudden death.5 A number of
water-borne minerals were examined as potential cardiotoxic or
cardioprotective factors, and over the past few decades a
consensus has emerged that low Mg content in drinking water is
associated with high rates of sudden death.
Magnesium metabolism
Distribution and measurement. After potassium, Mg is
the most common intracellular cation. It is an important
component in a variety of biologic processes, and it is critical
for the actions of many enzymes. Mg is distributed throughout the
body as follows: approximately two thirds is located in bone,
close to one third is intracellular, and the rest is
extracellular.6, 7 A 70 kg adult contains about 2000
mEq of Mg (1 mEq = 0.5 mmol = 12 mg), and normal serum values
vary between 1.5 and 2.5 mEq/L.8
Because the blood contains less than 1% of total body Mg
stores, serum Mg is poorly reflective of whole body levels.
However, although normal serum levels may be seen in the setting
of Mg deficiency, if serum levels are low, Mg deficiency is
usually present.7-9 Sophisticated means have been
developed to assess total body Mg stores,7, 10 but
these techniques are not commonly available, and they have been
used in very few studies.
Nutritional sources. The body’s Mg requirements
have been estimated to range from 18 to 33 mEq/day, while average
intake in the United States has been estimated to range from 20
to 30 mEq/day.6-7, 11 Because average intake is so
close to requirement levels, nutrition surveys suggest that
dietary Mg is often barely adequate to meet daily
requirements.11, 12 Foods rich in Mg include nuts,
cereals, seafoods, and green leafy vegetetables.8, 13
Boiling these foods in Mg-deficient soft water may leach out Mg,
while boiling in Mg-rich hard water may prevent its
loss.14 In addition, gut absorption of water-borne Mg
may be more efficient than that of food-borne Mg. Consequently,
Mg bioavailability may be greater from water than from food
sources.15 Because of the marginal intake and
absorption of Mg from food sources, it has been estimated that in
hard water areas, 20% to 40% of a person’s daily Mg
requirements may be provided by the Mg contained in drinking
water.16
Water hardness. Magnesium and calcium (Ca) are the
principal minerals that determine water hardness, but the
proportions of these minerals may vary
substantially.17 In North America, Mg:Ca ratios
generally range from 1:1 to 1:5, but in certain areas of Western
Europe, they may be two orders of magnitude lower.18
Knowledge of Mg and Ca contributions to water hardness is
important when assessing studies relating Mg deficiency and
sudden death. In many of the early epidemiologic studies, exact
mineral content was not reported, and this presents a problem
when trying to evaluate these studies.
Magnesium deficiency and sudden death
Epidemiologic studies. In the late 1950s and early
1960s, evidence began to accumulate documenting striking
geographic differences in the incidence of cardiovascular
disease. Cardiovascular disease was shown to be more common in
areas with increased mineral content in drinking water. The
relationship was first described by Kobayashi3 in
Japan, and shortly thereafter by Schroeder4 in the
United States. Kobayashi’s findings related stroke
incidence and the acidity of river water. Schroeder subsequently
analyzed regional incidences of cardiovascular disease and found
an inverse relationship with water hardness.
In the 1960s and early 1970s, Anderson et al.5, 19
conducted a series of studies in Ontario, Canada. Since there is
a gradient of water hardness across Ontario, these investigators
examined the incidence of acute and nonacute ischemic heart
disease in hard and soft water areas. Little relationship was
found with nonacute heart disease, but an inverse relation ship
was found between water hardness and sudden death. In hard water
areas (water hardness >200 ppm), the standardized death rate
from ischemic heart disease was 365 in 100,000, and 120 in
100,000 of these deaths were sudden. In soft water areas (water
hardness <100 ppm), the death rate was 416 in 100,000, and 195
deaths in 100,000 were sudden. Among deaths ascribed to heart
disease, the proportion of sudden deaths was 20% to 30% higher in
soft water areas compared with death rates in hard water
areas.
Following these early reports, epidemiologic studies in a
number of countries confirmed the inverse relationship between
drinking water hard ness and sudden death, while a few reports
found no correlation.20-27 (The lack of correlation
between water hardness and sudden death in several reports was
later explained by the inclusion of hard water areas with
unusually low Mg concentrations.) Although analytical techniques
were different among the studies, several found similar
correlation coefficients between water hardness and
cardiovascular disease (-0.59 to -0.70), and others found that
cardiovascular mortality or sudden death was at least 10% more
common in soft water areas than in hard water areas.
Once a relationship between water hardness and sudden death
was established, investigators examined whether it was the result
of a cardiotoxic factor in soft water or a cardioprotective
factor in hard water. Initially, a cardiotoxic factor was
suspected, because it was known that soft water can leach out
undesirable minerals from pipes and geologic layers.28
No strong correlations were found when a variety of minerals was
examined, however, and a cardioprotective factor began to be
suspected. Many elements were investigated, with attention
focusing on Mg and Ca because of their importance in deter mining
water hardness. Mg was found to correlate most closely (in an
inverse fashion) with sudden death rates.29, 30
Autopsy studies. Autopsy data were next examined in
an effort to link intracellular Mg levels with drinking water
intake and sudden death. Investigators were particularly
interested in myocardial Mg content. Anderson et al.31
examined myocardial tissue from people dying of trauma in hard
and soft water areas. Myocardial Mg content was significantly
lower in people living in soft water areas compared with levels
in people living in hard water areas (207 versus 222 µg/gm
wet weight, respectively). These differences in Mg content were
only found in myocardial tissue samples; they were not present in
serum samples or in tissue samples from diaphragm or pectoralis
muscle.16
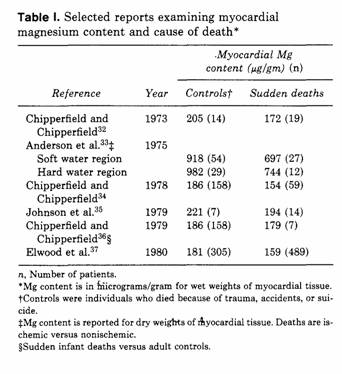
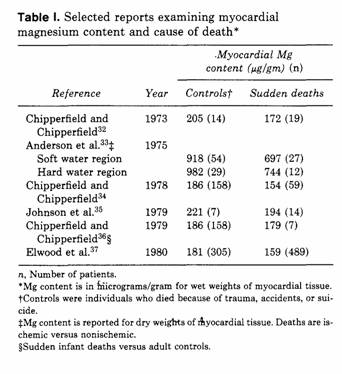
A series of studies also examined myocardial Mg content in
people dying of sudden death and in controls who died of trauma
(Table I).32-37 These studies consistently showed
depressed levels of myocardial Mg in people who died suddenly.
Although it is clear that myocardial Mg content is decreased
after sudden death, it is still unclear whether this is a cause
or an effect.
Animal and clinical studies. In conjunction with
epidemiologic and autopsy studies, animal and clinical studies
were also conducted. These studies suggest two possible
mechanisms for the association between Mg deficiency and sudden
death: arrhythmogenesis and coronary artery vasospasm. According
to the arrhythmogenesis theory, Mg deficiency in creases cardiac
irritability and facilitates cardiac arrhythmias.38
Experimental studies show that Mg is an essential cofactor for
Na-K adenosine triphosphatase (ATPase), an enzyme that influences
cardiac irritability by regulating ion fluxes across myocardial
cell membranes. Clinical reports40-42 suggest that Mg
deficiency is linked with cardiac rhythm disturbances including
premature ventricular beats, ventricular and supraventricular
arrhythmias, and torsades de pointes. These studies also suggest
that Mg deficiency lowers the threshold for digitalis-toxic
arrhythmias,43 and that intravenous Mg can acutely
reverse cardiac rhythm disturbances in some
situations.44-46
A second proposed mechanism is that Mg deficiency causes
coronary artery vasospasm, leading to myocardial ischemia and
sudden death. Evidence comes from several animal
studies47-49 in which vasospasm was induced by
Mg-deficient solutions and vasospasm subsequently resolved with
the addition of Mg. Other studies50, 51 have
documented pathologic changes in the heart associated with Mg
deficiency, and these changes have been linked with chronic
myocardial ischemia. Although these studies suggest that coronary
artery vasospasm induced by Mg deficiency may be responsible for
sudden death, complementary clinical data are lacking.
Magnesium
supplementation. The large number of studies that
suggest an association between Mg deficiency and sudden death
raise the issue of whether Mg supplementation can be used for the
primary prevention of sudden death. Several methods of
supplementation have been proposed including: public education to
change dietary habits, addition of Mg to community water
supplies, fortification of foods, and oral supplementation.
Before supplementation can be considered, however, several
questions need to be answered: (1) Will Mg supplementation reduce
the risk of sudden death? (2) How much time is required before
the effects of such supplementation are evident? (3) What is the
optimal method of supplementation? and (4) Is supplementation
technically and financially feasible?
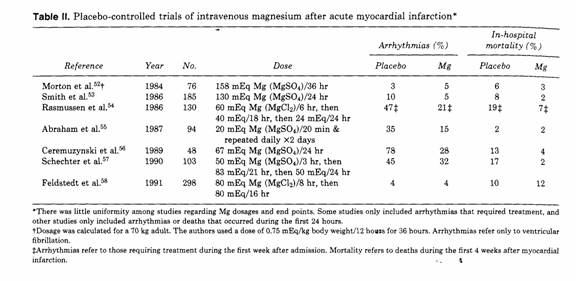
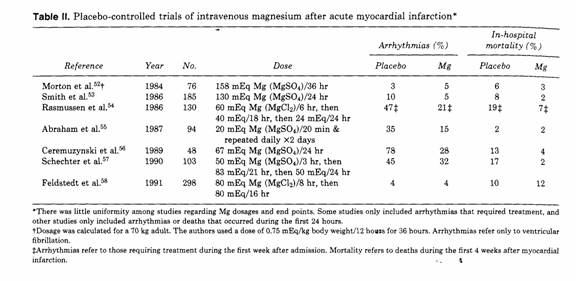
Risk reduction. Can Mg supplementation be used for
the primary prevention of sudden death? Although no studies have
addressed this question directly, a number of double-blind,
placebo-con trolled trials have examined the use of Mg
supplementation for secondary prevention. These studies examined
the efficacy of intravenous Mg supplementation in patients
hospitalized after myocardial infarction (Table II).52,
58 Most of these studies indicate that intravenous Mg
decreases the incidence of cardiac arrhythmias and overall
mortality after acute myocardial infarction. Although intravenous
Mg supplementation may be useful in patients at high risk for
ventricular arrhythmias, little research has been directed at
supplementation in people with long standing but mild Mg
deficiency (as might be expected in people living in soft water
areas). Nevertheless, results from the early epidemiologic
studies5, 22 suggest that sudden death rates in soft
water water areas are at least 10% greater than sudden death
rates in hard water areas. If Mg supplementation causes even a
modest decrease in sudden death rates a substantial number of
lives might be saved.
Timing of supplementation. If Mg supplementation
decreases the risk for sudden death, how long will it take before
the effects are seen? Then answer to this question will have an
impact on the choice of supplementation methods and the length of
time supplementation will need to be maintained. If sudden death
is related to intracellular Mg depletion, then supplementation
might be able to reverse the situation rather quickly. If sudden
death is related to pathologic changes caused by chronic Mg
deficiency, then supplementation may have to be given for many
years before a change in death rates is observed. One
study59 addressed this question tangentially by
observing changes in death rates following a change in the source
of community water supplies and coincidental increases in
drinking water hardness. Within a few years of drinking water
changes, reductions in death rates were evident. This study did
not quantify the Mg content of the drinking water, however, and
overall cardiovascular mortality was assessed rather than sudden
death. No interventional trials have yet addressed this
issue.
Methodology. What is the best method of increasing Mg
intake? One method is public health education to increase the use
of Mg-rich hard water for drinking and cooking. Health education
could be used to discourage the use of water softeners to treat
water used for drinking and cooking. (Conventional water
softeners remove natural Mg.) At the same time, the consumption
of Mg-rich food and water could be encouraged.
A second method of supplementation is the addition of Mg to
community water supplies, similar to fluoridation. If Mg content
in soft water areas could be raised to levels found in hard water
areas, a drop in sudden death rates would be strong evidence that
supplementation makes a difference.
A third method of increasing Mg intake involves the
fortification of foods. In Finland, substitution of Mg for part
of the sodium in table salt was shown to be a safe way of
increasing Mg intake, and this substitution was associated with
an increase in serum Mg.60 Sudden death rates could
not be examined in this study because of the small number of
patients investigated.
Finally, oral Mg supplementation has been suggested for people
at high risk of sudden death. This type of supplementation would
be similar to potassium supplementation for cardiac patients who
are receiving diuretics. The advantages of oral supplementation
over other methods are that it is cheap and that it can be easily
targeted at high-risk groups. In addition, oral Mg has long been
prescribed by clinicians who were influenced by the early
epidemiologic studies. With the exception of hypermagnesemia in
patients with renal failure, few adverse effects have been
reported. Although large-scale clinical trials have not yet been
attempted, the long history of oral Mg supplementation testifies
to its safety.
Feasibility. Is Mg supplementation feasible? Public
health education to increase Mg intake is unlikely to be
controversial, but the questions of how to supplement Mg and in
whom remain unanswered. Large-scale Mg supplementation of
community water supplies is impractical because of technologic
and political obstacles.18, 61 Fortification of foods
is technically feasible and would be less controversial, since
many foods are now fortified with vitamins and minerals. To date,
however, oral Mg is the best studied of the alternatives and
might well be the most feasible initial intervention. Patient
acceptability, low cost, and the possibility of targeting
high-risk groups make this an easy method to implement and
monitor.
Conclusions.
Substantial evidence suggests that Mg deficiency is associated
with sudden death, but most data come from observational rather
than interventional studies. Proof that Mg supplementation
reduces the risk of sudden death is needed before efforts to
increase Mg intake are undertaken. Sufficient data have
accumulated to justify a large, randomized, placebo-controlled
trial for the primary prevention of sudden death. If such a study
demonstrates that Mg supplementation reduces both sudden death
and overall mortality rates, then large-scale efforts may be
warranted.
Summary.
A link between Mg deficiency and sudden death is suggested by a
substantial number of studies published over the past three
decades. Data come from epidemiologic, autopsy, clinical, and
animal studies. They suggest that: (1) Sudden death is common in
areas where community water supplies are Mg-deficient. (2)
Myocardial Mg content is low in people who die of sudden death.
(3) Cardiac arrhythmias and coronary artery vasospasm can be
caused by Mg deficiency and (4) Intravenous Mg reduces the risk
of arrhythmia and death immediately after acute myocardial
infarction. Because of these data, Mg supplementation has been
proposed as a possible method of reducing the risk of sudden
death. Suggested ways of supplementing Mg include public
education to change dietary habits, addition of Mg to community
water supplies, fortification of foods, and oral supplementation.
Despite the substantial number of studies linking Mg deficiency
with sudden death, no prospective studies have yet investigated
whether large-scale Mg supplementation is useful for the primary
prevention of sudden death.
I thank Mr. John Marier (National Research Council of Canada),
Dr. Dade Moeller (Harvard School of Public Health), and Dr.
Kenneth Flegel (Royal Victoria Hospital, McGill University) for
many helpful suggestions.
REFERENCES
1. Zipes DP. Sudden cardiac death. In: Wyngaarden JB, Smith
LH, Bennett JC, eds. Cecil textbook of medicine. 19th ed.
Philadelphia: WB Saunders Company, 1992:250-3.
2. Lown B. Sudden cardiac death: the major challenge
confronting contemporary cardiology. Am J Cardiol
1979;43:313-28.
3. Kobayashi J. Geographic relationship between the chemical
nature of river water and death-rate from apoplexy. Ber Ohara
Inst Landwirt Biol 1957;11:12-21.
4. Schroeder HA. Relation between mortality from
cardiovascular disease and treated water supplies. JAMA 1960;172:
1902-8.
5. Anderson TW, LeRiche WH, MacKay JS. Sudden death and
ischemic heart disease: correlation with hardness of local water
supply. N Engl J Med 1969;280:805-7.
6. Cronin RE, Knochel JP. Magnesium deficiency. Adv Intern Med
1983;28:509-33.
7. Dirks JH, Alfrey AC. Normal and abnormal magnesium
metabolism. In: Schrier RW, ed. Renal and electrolyte disorders.
3rd ed. Boston: Little, Brown & Company, 1986:331-59.
8. Assessment and oral management of micronutrient deficiency.
In: Alpers DH, Clouse RE, Stenson WF, eds. Manual of nutritional
therapeutics. 2nd ed. Boston: Little, Brown & Company,
1988:90-4.
9. Alfrey AC, Miller NL, Butkus D. Evaluation of body
magnesium stores. J Lab Clin Med 1974;84:153-62.
10. Rasmussen HS, McNair P, Goransson L, Balslov S, Larsen OG,
Aurup P. Magnesium deficiency in patients with ischemic heart
disease with and without acute myocardial infarction uncovered by
an intravenous loading test. Arch Intern Med 1988;
148:329-32.
11. Jones JE, Manalo R, Funk EB. Magnesium requirements in
adults. Am J Clin Nutr 1967;20:632-5.
12. Seelig MS. The requirement of magnesium by the normal
adult: summary and analysis of published data. Am J Clin Nutr
1964;14:342-90.
13. Marier JR. Magnesium content of the food supply in the
modern day world. Magnesium 1986;5:1-8.
14. Haring BSA, van Delft W. Changes in the mineral
composition of food as a result of cooking in "hard" and "soft"
waters. Arch Environ Health 1981;36:33-5.
15. Lowik MRH, Groot EH, Binnerts WT. Magnesium and public
health: the impact of drinking water. In: Hemphill DD, ad. Trace
substances in environmental health. vol 16. Columbia, Missouri:
University of Missouri, 1982:189-95.
16. Anderson TW, Leriche WH, Hewitt D, Neri LC. Magnesium,
water hardness, and heart disease. In: Cantin M, Seelig MS, eds.
Magnesium in health and disease. New York: SP Medical and
Scientific Books, 1980:565-71.
17. Water hardness and cardiovascular disease. In: Drinking
water and health. vol 3. Safe Drinking Water Committee. National
Academy of Sciences. Washington, DC: National Academy Press,
1980:21-4.
18. Durlach J, Bara M, Guiet-Bara A. Magnesium level in
drinking water and cardiovascular risk factor: a hypothesis.
Magnesium 1985;4:5-15.
19. Anderson TW, LeRiche WH. Sudden death from ischemic heart
disease in Ontario and its correlation with water hardness and
other factors. Can Med Assoc J 1971;105:155-60.
20. Schroeder HA. Municipal drinking water and cardiovascular
death rates. JAMA 1966;195:125-9.
21. Crawford MD, Gardner MJ, Morris JN. Mortality and hardness
of local water supplies. Lancet 1968;1:827-31.
22. Peterson DR, Thompson DJ, Nam JM. Water hardness,
arteriosclerotic heart disease and sudden death. Am J Epidemiol
1970;92:90-3.
23. Neri LC, Hewitt D, Mandel JS. Risk of sudden death in soft
water areas. Am J Epidemiol 1971;94:101-4.
24. Punsar 5, Karvonen MJ. Drinking water quality and sudden
death: observations from West and East Finland. Cardiology
1979;64:24-34.
25. Pocock SJ, Shaper AG, Cook DG, et al. British regional
heart study: geographic variations in cardiovascular mortality,
and the role of water quality. Br Med J 1980;280:1243-9.
26. Luoma H, Aromaa A, Helminen 5, et al. Risk of myocardial
infarction in Finnish men in relation to fluoride, magnesium and
calcium concentration in drinking water. Acta Med Scand 1983;213:
17 1-6.
27. Lacey RF, Shaper AG. Changes in water hardness and
cardiovascular death rates. Int J Epidemiol 1984;13:18-24.
28. Schroeder HA, Kraemer LA. Cardiovascular mortality,
municipal water, and corrosion. Arch Environ Health
1974;28:303-11.
29. Allen HAJ. An investigation of water hardness, calcium,
and magnesium in relation to mortality in Ontario. PhD Thesis.
University of Waterloo, Ontario, Canada, 1972.
30. Karppanen H. Epidemiological studies on the relationship
between magnesium intake and cardiovascular diseases. Artery
1981;9:190-9.
31. Anderson TW, Hewitt D, Neri LC, Schreiber G, Talbot F.
Water hardness and magnesium in heart muscle (Letter). Lancet
1973;2:1390-1.
32. Chipperfield B, Chipperfield JR. Heart-muscle magnesium,
potassium, and zinc concentrations after sudden death from
heart-disease. Lancet 1973;2:293-6.
33. Anderson TW, Neri LC, Schreiber GB, Talbot FDF, Zdrojewski
A. Ischemic heart disease, water hardness and myocardial
magnesium. Can Med Assoc J 1975;113:199-203.
34. Chipperfield B, Chipperfield JR. Differences in metal
content of the heart muscle in death from ischemic heart disease.
AM HEART J 1978;95:732-7.
35. Johnson CJ, Peterson DR, Smith EK. Myocardial tissue
concentrations of magnesium and potassium in men dying suddenly
from ischemic heart disease. Am J Clin Nutr 1979;32:967-70.
36. Chipperfield B, Chipperfield JR. Cot deaths and mineral
salts (Letter). Lancet 1979;1:220.
37. Elwood PC, Sweetnam PM, Beasley WH, Jones D, France R.
Magnesium and calcium in the myocardium: cause of death and area
differences. Lancet 1980;2:720-2.
38. Eisenberg MJ. Magnesium deficiency and cardiac
arrhythmias. NY State J Med 1986;86:133-6.
39. Skou JC, Butler KW, Hansen O. The effect of magnesium,
ATP, Pi, and sodium on the inhibition of the (Na+ +
K+) activated enzyme system by g-strophanthin. Biochim
Biophys Acta 1971;241:443-61.
40. Chadda KD, Lichstein E, Gupta P. Hypomagnesemia and
refractory cardiac arrhythmia in a nodigitalized patient. Am J
Cardiol 1973;31:98-100.
41. Loeb HS, Pietras RJ, Gunnar RM, Tobin JR Jr. Paroxysmal
ventricular fibrillation in two patients with hypomagnesemia.
Circulation 1968;37:210-5.
42. Topol EJ, Lerman BB. Hypomagnesemic torsades de pointes.
Am J Cardiol 1983;52:1367-8.
43. Seller RH, Cangiano J, Kim KE, Mendelssohn S, Brest AN,
Swartz C. Digitalis toxicity and hypomagnesemia. AM HEART J
1970;79:57-68.
44. Iseri LT, Chung P, Tobis J. Magnesium therapy for
intractable ventricular tachyarrhythmias in normomagnesemic
patients. West J Med 1983;138:823-8.
45. Cohen L, Kitzes R. Magnesium sulfate and digitalis-toxic
arrhythmias. JAMA 1983;249:2808-10.
46. Tzivoni D, Keren A, Cohen AM, et al. Magnesium therapy for
torsades de pointes. Am J Cardiol 1984;53:528-30.
47. Altura BM, Altura BT. Magnesium and vascular tone and
reactivity. Blood Vessels 1978;15:5-16.
48. Turlapaty PDMV, Altura BM. Magnesium deficiency produces
spasms of coronary arteries: relationship to etiology of sudden
death ischemic heart disease, Science 1980;208:198-200.
49. Altura BM, Altura BT. Magnesium ions and contraction of
vascular smooth muscles: relationship to some vascular diseases.
Fed Proc 1981;40:2672-9.
50. Crawford T, Crawford MD. Prevalence and pathological
changes of ischaemic heart-disease in a hard-water and in a
soft-water area. Lancet 1967;1:229-332.
51. Altura BM. Sudden-death ischemic heart disease and dietary
magnesium intake: is the target site coronary vascular smooth
muscle? Med Hypotheses 1979;5:843-8.
52. Morton BC, Nair RC, Smith FM, McKibbon TG, Poznanski WJ.
Magnesium therapy in acute myocardial infarction—a
double-blind study. Magnesium 1984;3:346-52.
53. Smith LF, Heagerty AM, Bing RF, Barnett DB. Intravenous
infusion of magnesium sulphate after acute myocardial infarction:
effects on arrhythmias and mortality. Int J Cardiol
1986;12:175-80.
54. Rasmussen HS, McNair P, Norregard P, Backer V, Lindeneg O,
Balslev S. Intravenous magnesium in acute myocardial infarction.
Lancet 1986;1:234-6.
55. Abraham AS, Rosenmann D, Kramer M, et al. Magnesium in the
prevention of lethal arrhythmias in acute myocardial infarction.
Arch Intern Med 1987;147:753-5.
56. Ceremuzynski L, Jurgiel R, Kulakowski P, Gebalska J.
Threatening arrhythmias in acute myocardial infarction are
prevented by intravenous magnesium sulfate. AM HEART J
1989;118:1333-4.
57. Schechter M, Hod H, Marks N, Behar S, Kaplinsky E,
Rabinowitz B. Beneficial effect of magnesium sulfate in acute
myocardial infarction. Am J Cardiol 1990;66:271-4.
58. Feldstedt M, Boesgaard 5, Bouchelouche P, et al. Magnesium
substitution in acute ischaemic heart syndromes. Eur Heart J
1991; 12: 12 15-8.
59. Crawford MD, Gardner MJ, Morris JN. Changes in water
hardness and local death-rates. Lancet 1971;2:327-9.
60. Karppanen H, Tanskanen A, Tuomilehto J, et al. Safety and
effects of potassium- and magnesium-containing low sodium salt
mixtures. J Cardiovasc Pharmacol 1984; 6(suppl 1):S236-43.
61. Marier JR, Neri LC, Anderson TW. Water hardness, human
health, and the importance of magnesium. Monograph No. 17581.
Ottawa: National Research Council of Canada, 1979:92.
From the Cardiology Division of the Department of Medicine,
University of California, San Francisco.
Received for publication Dec. 30, 1991; accepted March 3,
1992.
Reprint requests: Mark J. Eisenberg, MD, Moffitt-Long
Hospital/Box 0214, University of California, 505 Parnassus Ave.,
San Francisco, CA 94143.
This page was first uploaded to The Magnesium Web Site on
August 22, 2002
http://www.mgwater.com/